Gene-Edited Islet Cells Show Promise for Type 1 Diabetes Treatment
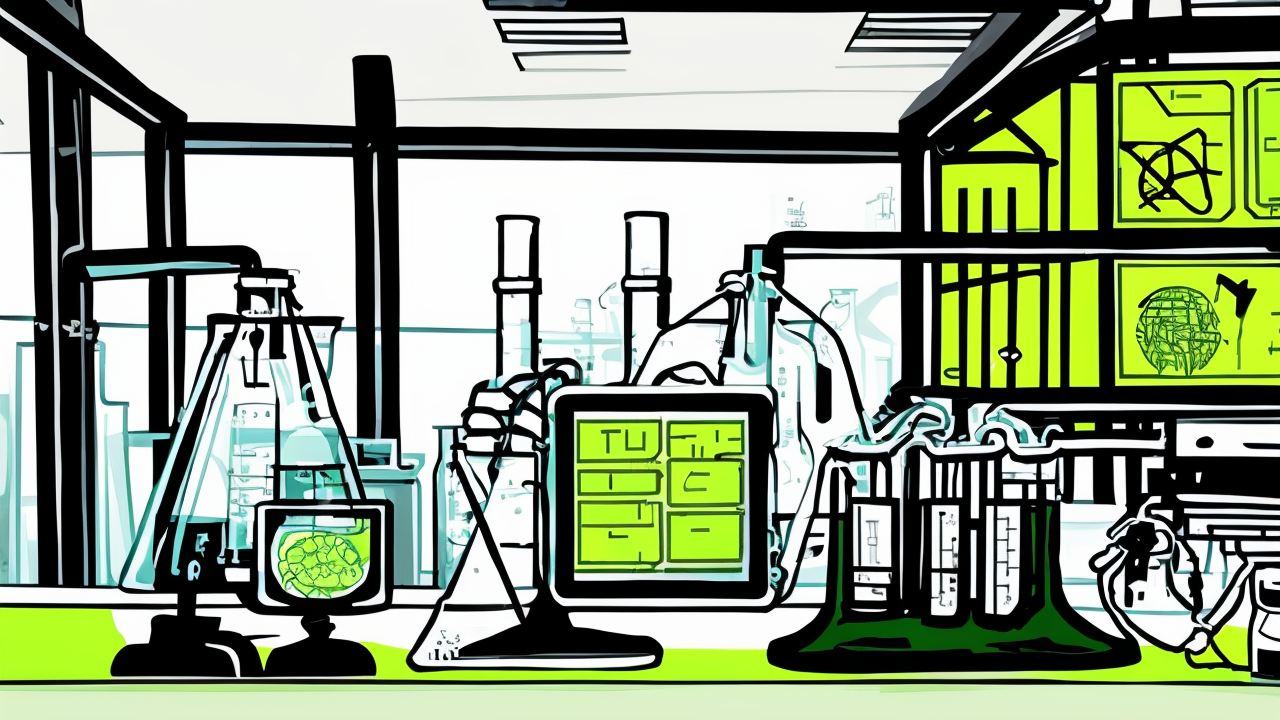
In a groundbreaking first-in-human study, a 42-year-old man with type 1 diabetes (T1D) successfully produced his own insulin after receiving gene-edited islet cell transplantation without immunosuppression. The procedure utilized UP421, a gene-edited hypoimmune platform (HIP) developed by Sana Biotechnology, to avoid immune rejection.
The patient, who had lived with T1D for 37 years, experienced a 42% reduction in HbA1c levels and stable, glucose-responsive insulin secretion within 12 weeks. His immune system did not mount a response against the gene-edited cells, marking a significant advancement in treating T1D.
The islet cells, derived from a deceased donor, were edited using CRISPR-Cas12b and lentiviral transduction to reduce immunogenicity. Transplanted into the patient’s forearm muscle, the cells survived and functioned without the need for immunosuppressive drugs.
“This approach represents a potential paradigm shift in treating T1D,” said lead researcher Per-Ola Carlsson, MD, PhD, of Uppsala University. “By enabling immune evasion, we may circumvent the need for lifelong immunosuppression, offering a more practical and safer treatment option.”
While the results are promising, longer-term follow-up is needed to confirm the efficacy, safety, and durability of this approach. The study was published in the New England Journal of Medicine and funded by the Leona M. and Harry B. Helmsley Charitable Trust.
Experts caution that the reliance on deceased donor islets may limit broader application, but ongoing research into stem cell-derived islets could address this limitation. If successful, this method could revolutionize diabetes care by offering a functional cure without the risks associated with immunosuppression.
Published: 8/4/2025